I’m not as big a conference attendee like some people I know (Ed – you mean @EMManchester), but when I heard the conference had its own Spotify playlist (featuring the Matrix soundtrack) and saw the welcome banner, I got the feeling that #TactT19 wasn’t going to be like any other conferences I’d been to before in my (admittedly) limited experience.
Tactical Trauma 2019 was an international conference based in Sundsvall, Sweden on pre-hospital trauma and critical care with a tactical twist. It brought to the conference some world-class speakers working with pre-hospital trauma in a tactical/hostile environment. Physicians, EMS, police anti-terror units, military, fire and rescue service were all represented. It was a fascinating conference and I’m going to share some of the #FOAMed gems I learned.
Day one opened with a talk from Jeff Yost who was an off duty paramedic during the Las Vegas shooting in October 2017.
Despite being set up for the minor injuries and dehydration that they expected to see at the Country and Western concert, Jeff ensured that all injured patients had a volunteer bystander with them to stay with them and inform the trained staff of any changes – vital in a mass casualty situation where you are overwhelmed by casualties. Seventy ‘off duty’ responders helped during that time.

Over 800 people were injured in the attack. 413 had gunshot wounds and many more were injured in the stampede to get away. Patients ran to safety and then called for help leading the police to wrongly believe that attacks were taking place over the city.
Lots of food for thought… how many tourniquets do you need for a 50,000 person event? How do we train the public to assist in mass casualties when there is a responder vacuum? In a military setting everyone is trained to assist in a mass casualty setting but how can we transfer this to civilian life? What’s the best way of getting mass casualties to hospitals? During the Las Vegas attack patients were taken by private cars, taxis, fences and even bins.
Second up was the excellent Michael Lauria talking about Emergency Reflex Action Drills. I can’t do it justice here so check out the article at EMCrit1
Lots of great ideas taken from military training that you can take back and put into practice in your resus rooms.
Studies suggest we have to do something 60-100 times before it becomes a habit. During stressful situations you struggle to make decisions and can’t take in information so make up an ERAD for something you commonly do that is time critical e.g RSI. Practise over and over until it becomes instinctive. Bottom line – train like you fight, fight like you train.
Mark Forrest gave a great talk on the latest evidence for major haemorrhage control. It started with a sobering reminder that 90% of deaths from major haemorrhage occur in the first 24 hours but we still fail to identify and control bleeding. There was a review of the evidence for haemostatic dressings- they all seem to work but L-arginine may be the best2.
One particularly exciting new development to watch for the future is UV activated hydrogel which has shown promise in animal studies3.
My take home point was that despite all the latest dressings, gels or tourniquets, direct pressure can control 90% of bleeds 4 and that again training the public may be the best strategy from time zero.
Impact brain apnoea is a topic dear to our hearts at St Emlyns 5. Mark Wilson creator of the GoodSAM App (go and download it now!) regularly gives a great talk on the topic, and this time was no exception. A couple of key points – alcohol seems to extend the apnoeic time period. 80% of patients in RTCs who bullseyed the windscreen had a brain injury and this risk was even higher if blood or hair was on the windscreen – so really take note at paramedic handover and listen to what they have to say.
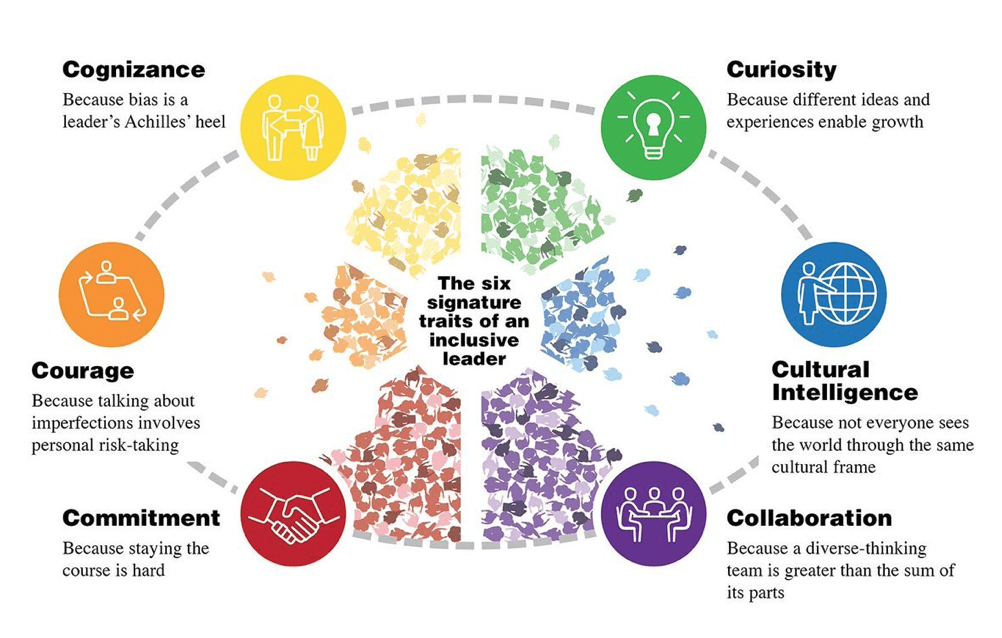
Kate Prior gave us a talk on how we can be better leaders, and in particular inclusive leaders.
We all have inherent bias and being aware of them can help us with this. Check out this this free tool to see which yours might be,and check out the St Emlyn’s blog in how this affects us in the ED6.
She then talked about imposter syndrome, which is something that most of us (70% according to studies) suffer from at some point in our lives/careers. We can feel like a fraud, create a reason to support that belief, work to correct it, feel good temporarily but then feel like a fraud again. Suggested ways to combat this were to get a mentor and challenge our negative thoughts before they become repetitive.

Mike Clumpner ( see his site at www.threatsuppression.com) was one of the fastest and most engaging speakers I’ve heard in a long time. He introduced a new concept to me of fire as a weapon in mass casualty situations where a fire is deliberately started to complicate an already deadly situation.
It was frightening to hear how terrorist organisations publish guidance on how to use fire as a weapon and ways to counteract the emergency response to fires. Fire has been used in several terrorist attacks, we can’t say we haven’t been warned, but are we ready for it and do we have a plan?
One of my personal highlights of the conference was a talk by Greg Ciottone – a man who literally wrote the book on disaster medicine. Greg lead the first response team at 9/11 and bravely talked about his experiences with PTSD and how we need to care for ourselves and our teams. It was particularly poignant in light of the fact that over 2000 responders to the 9/11 attacks have died in the time since.
Closing out day 1 was Mike Abernethy. His talk ‘Police drop offs in penetrating trauma. Are you serious?’ presented evidence why this isn’t as crazy as first appears7,8.
Big questions we need to consider:
- Does the patient get to definitive care quicker than they would with an ambulance?
- Should we use the public to help and if so how do we do this?
- The eternal debate of stay and play vs scoop and run
- Is there truly a time critical injury?
- Does the patient need treatment before hospital to make it to hospital / interventions on route?
Opening day 2 was Michael Lauria on the essence of Tactical Medicine summed up as:
- Speed – take the patient where they need to go quickly if you’re near to a hospital, if you can’t do what you can in the field
- Simplicity – does it work or not?
- Coordination of care – we are not the mission, we are a small part of it.
Doing these things well will improve care for our patients. My take home point was that it’s essential that we’re doing the basics well before going on to the marginal gains that we can obsess over and distract us from doing the simple things. It reminded me of a great piece of advice I received when I was a medical student from a cardiologist called Dr Phil Lewis who told me about his concept of doing the ‘ordinary things excellently’.
The traditional concept of emergency triage was challenged throughout the conference and particularly in the second talk by Mike Clumpner entitled Best Practice at Mass Casualty Events. Key points raised were:
- In a review of 100 active shooter events in the USA death or serious injury occurs every 15 seconds (or maybe less)9.
- In mass casualty situations the public need to get down and hide quickly as advised by the UK government.
- The cycle of disaster begets disaster- for example in the Las Vegas shooting people run and then get injured in the crush. Are we ready and prepared for the secondary injuries?
- If a victim sustains a serious but survivable injury their mortality increases by 2-4%/minute until they get to theatre or receive blood products. Time is certainly of the essence10,11,12
Mike introduced the concept of the ‘time thief’ in mass casualties. Anything that takes us away from these priorities…
- Rapid recognition and control of life threatening haemorrhage.
- Getting people away from the ‘hot zone’
- Triage with prioritisation of patients with internal bleeding
…is a ‘time thief’ and Mike quoted the Pulse nightclub shooting as an example13 of 16 patients who died from potentially survivable wounds.
One further point that he made was that traditional triage tagging may delay life saving interventions.
Maybe it’s time to think about having dedicated dual roles of triage/tagging and another person doing haemorrhage control? What do you all think?
I’ll admit I’m not a big dog lover (please don’t hate me – I was bitten as a child!) but there was a fascinating talk on injured police dogs that I’ll summarise for the animal lovers out there. If your dog is injured you should muzzle it (for everyone’s safety) as dogs in pain bite! IM morphine is the drug of choice. Ketamine is not recommended because of hypersalivation and agitation (is this finally the one time when we don’t use ketamine?). In terrorist incidents using dogs to search for bombs, if the dog gets hot and starts panting they can’t smell for explosives so may need an ice bath to cool down before returning to sniffing duty.
Miretta Tomilla was a doctor who did her first resucitative hysterotomy in the field. She presented on two cases of babies surviving neurologically intact after the procedure. The key is to remember that you are doing the hysterotomy primarily to save the mother as delivering the baby increases cardiac output 60-80%. Something that we may think is futile sometimes has a good outcome14.
Everyone gets quite twitchy with burns and especially to the face but are we doing too many intubations? Possibly so. Knut Taxbro presented the evidence on this15.
The closing talk of the conference was on intentional vehicular assault by Faizan Arshad. Patients in these incidents typically have higher ISS than other non-intentional vehicle incidents. The scene of these incidents could be over a large area such as in Nice, leading to difficult decisions on where to send ambulances and resources. Again, prevention and empowering the public to help are key to reducing deaths.
The closing words from Fredrik Granholm – ‘Be great and inspire others’ are something we all want to carry on to our places of work.
Thanks for reading. It’d be great to read your comments below.
Pete @tropdocpete
References
- 1.Weingart S. Emergency Reflex Action Drills. EMCRIT. https://emcrit.org/emcrit/emergency-reflex-action-drills/. Published 2018. Accessed October 2019.
- 2.Rembe J-D, Böhm JK, Fromm-Dornieden C, et al. Comparison of hemostatic dressings for superficial wounds using a new spectrophotometric coagulation assay. J Transl Med. November 2015. doi:10.1186/s12967-015-0740-5
- 3.Hong Y, Zhou F, Hua Y, et al. A strongly adhesive hemostatic hydrogel for the repair of arterial and heart bleeds. Nat Commun. May 2019. doi:10.1038/s41467-019-10004-7
- 4.Slevin JP, Harrison C, Da Silva E, White NJ. Martial arts technique for control of severe external bleeding. Emerg Med J. January 2019:154-158. doi:10.1136/emermed-2018-207966
- 5.Carley S. PODCAST update with Mark Wilson on the GoodSAM app at the London Trauma Conference. St Emlyn’s. https://www.stemlynsblog.org/podcast-update-mark-wilson-goodsam-app-london-trauma-conference/. Published 2015. Accessed 2019.
- 6.Carley S. Do Emergency Physicians judge patients on race, sex, sexual orientation, weight, etc.? St. Emlyn’s. St Emlyn’s. https://www.stemlynsblog.org/most-emergency-physicians-judge-patients-on-race-sex-sexual-orientation-weight-st-emlyns/. Published 2013. Accessed October 2019.
- 7.Rubens JH, Ahmed OZ, Yenokyan G, Stewart D, Burd RS, Ryan LM. Mode of Transport and Trauma Activation Status in Admitted Pediatric Trauma Patients. Journal of Surgical Research. February 2020:153-159. doi:10.1016/j.jss.2019.08.008
- 8.Wandling MW, Nathens AB, Shapiro MB, Haut ER. Association of Prehospital Mode of Transport With Mortality in Penetrating Trauma. JAMA Surg. February 2018:107. doi:10.1001/jamasurg.2017.3601
- 9.peppers shawn. The Strategic Citizen: A Physical Security Model for Strategic Critical Infrastructure Protection (CIP). Journal of Physical Security. http://310g.on.uvu.edu/files/2016/12/The-Strategic-Citizen.pdf. Published 2010. Accessed October 2019.
- 10.Linkous D, Carter K. Responding to the shootings at Virginia Tech: planning and preparedness. J Emerg Nurs. 2009;35(4):321-325. https://www.ncbi.nlm.nih.gov/pubmed/19591726.
- 11.Kaplowitz L, Reece M, Hershey J, Gilbert C, Subbarao I. Regional health system response to the Virginia Tech mass casualty incident. Disaster Med Public Health Prep. 2007;1(1 Suppl):S9-13. https://www.ncbi.nlm.nih.gov/pubmed/18388622.
- 12.Crandall M, Sharp D, Unger E, et al. Trauma Deserts: Distance From a Trauma Center, Transport Times, and Mortality From Gunshot Wounds in Chicago. Am J Public Health. June 2013:1103-1109. doi:10.2105/ajph.2013.301223
- 13.Smith ER, Shapiro G, Sarani B. Fatal Wounding Pattern and Causes of Potentially Preventable Death Following the Pulse Night Club Shooting Event. Prehospital Emergency Care. April 2018:662-668. doi:10.1080/10903127.2018.1459980
- 14.Tommila M, Pystynen M, Soukka H, Aydin F, Rantanen M. Two cases of low birth weight infant survival by prehospital emergency hysterotomy. Scand J Trauma Resusc Emerg Med. July 2017. doi:10.1186/s13049-017-0407-8
- 15.Badulak JH, Schurr M, Sauaia A, Ivashchenko A, Peltz E. Defining the criteria for intubation of the patient with thermal burns. Burns. May 2018:531-538. doi:10.1016/j.burns.2018.02.016


Pingback: October 2019 Podcast round up. St Emlyn's • St Emlyn's