This podcast was originally recorded during the COVID 19 pandemic, but has many top tips about staying healthy in none pandemic times.
As healthcare workers continue to battle the COVID-19 pandemic, maintaining their own health and well-being is paramount. To provide practical advice and strategies, we’ve brought together two experts in sports medicine and nutrition. John Rogers, a consultant in Sport and Exercise Medicine, and Nathan Lewis, a nutrition scientist, share their insights on how to optimize sleep, manage stress, and enhance nutrition. By applying principles used by elite athletes, healthcare professionals can bolster their immune systems and stay resilient during these challenging times. Read on to discover evidence-based tips for staying healthy amidst the demands of the pandemic.
Listening Time: 31:24
The Current Challenge
As we face the COVID-19 pandemic, healthcare workers are experiencing unprecedented stress and pressure. Our workforce is not only battling the virus but also trying to maintain their own health. We need to flatten two curves: the infection curve among the general population and the infection curve among healthcare workers. If too many healthcare workers fall ill simultaneously, it could lead to a critical shortage of staff to care for patients.
The Importance of Sleep
John emphasizes the importance of sleep for immune health. Professional athletes aim for at least seven hours of sleep per night, and the same should apply to healthcare workers. Good sleep hygiene is crucial: minimize caffeine intake in the afternoon and evening, reduce screen time before bed, and ensure your sleeping environment is comfortable and dark.
Matthew Walker’s book, “Why We Sleep,” offers valuable insights into the importance of sleep. He suggests that caffeine and alcohol can disrupt sleep patterns, and shift workers should adopt strategies to mitigate these effects. Using sleep masks, earplugs, and establishing a regular pre-sleep routine can help improve sleep quality.
Managing Stress
Stress management is another critical area. High stress levels can weaken the immune system, making you more susceptible to infections. Strategies to reduce stress include regular exercise, meditation, and mindfulness practices. Apps like Calm and Headspace can provide guided meditation sessions, and online yoga classes can help with relaxation.
Professional sports teams have seen the benefits of mindfulness and meditation, and these practices can be equally beneficial for healthcare workers. Regular exercise, even just 30-60 minutes a day, can also help manage stress and improve overall health.
Nutrition and Immune Health
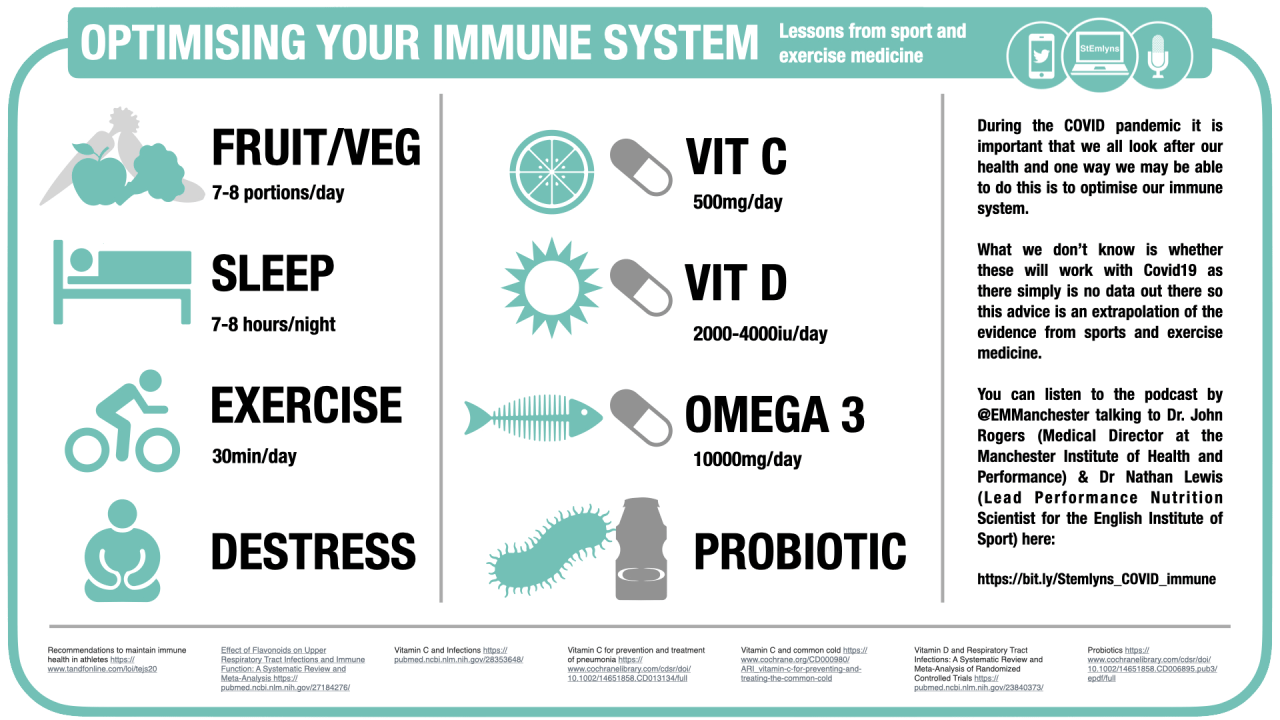
Nathan highlights the role of nutrition in maintaining a healthy immune system. Key nutrients like vitamin C, vitamin D, and omega-3 fatty acids are essential for immune function.
Vitamin C
Vitamin C has been shown to reduce the incidence of respiratory infections, especially in people under heavy physical stress. A Cochrane review found a 50% decrease in upper respiratory tract infections with vitamin C supplementation. Aim for 200-250 milligrams per day through diet or supplements.
Polyphenols
Polyphenols, found in fruits, vegetables, tea, and coffee, have also been shown to reduce respiratory infections. A meta-analysis showed a 30% reduction in upper respiratory tract infections with polyphenol intake. Strive for a diet rich in fruits and vegetables, aiming for seven to ten servings per day.
Vitamin D
Vitamin D is crucial, especially for those with limited sun exposure. Deficiency in vitamin D is common in northern climates, and supplementation can help maintain optimal immune function. Aim for 2,000-4,000 IU of vitamin D3 daily during winter months.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish, play a significant role in resolving inflammation. If you don’t consume fish regularly, consider supplements to ensure adequate intake of EPA and DHA.
Probiotics
Probiotics can also support immune health. A Cochrane review found a 50% decrease in respiratory infections with probiotic use. Consider probiotic drinks like Actimel and Yakult to support your immune system.
Practical Tips
- Sleep: Aim for seven hours of quality sleep per night. Minimize caffeine and alcohol intake, use sleep masks and earplugs, and establish a regular bedtime routine.
- Stress Management: Incorporate regular exercise, meditation, and mindfulness practices into your routine. Use apps like Calm and Headspace or participate in online yoga classes.
- Nutrition: Ensure your diet is rich in fruits, vegetables, and healthy fats. Consider supplements for vitamin C, vitamin D, omega-3 fatty acids, and probiotics if needed.
Conclusion
The COVID-19 pandemic presents unique challenges for healthcare workers. By adopting strategies from sports medicine and nutrition, we can maintain our health and well-being during these difficult times. Prioritize sleep, manage stress effectively, and ensure a nutritious diet to support your immune system. Stay safe and take care of yourselves as we navigate this crisis together.
For more detailed information and links to the studies mentioned, visit our blog and check out the resources provided by John and Nathan. Let’s work together to flatten both curves and keep our healthcare workforce healthy and ready to care for our patients.
Thank you for reading, and a special thank you to John and Nathan for sharing their expertise. Stay tuned for more updates and insights on the St Emlyn’s blog.
Contributors
Dr John Rogers is a Consultant in Sport & Exercise Medicine at Manchester University NHS Foundation Trust. He also works as Medical Director at the Manchester Institute of Health and Performance and as a Visiting Professor in Sport & Exercise Medicine at Manchester Metropolitan University. His previous jobs include CMO to British Triathlon, Institute Medical Officer to British Athletics, Consultant SEM Physician at the Defence Military Rehabilitation Centre, Headley Court, CMO for Team GB at Youth Olympic Games, Team Doctor for British Paralympic Athletics Team, Sports Physician at ORRECO and GP Partner at Brooklands Medical Practice. He has a particular clinical interest in medical problems related to endurance sport.
Dr Nathan A. Lewis currently works as the Lead Performance Nutrition Scientist for the English Institute of Sport (EIS), having worked as a senior performance nutritionist for the EIS across several Olympic cycles, including Beijing, London, Rio, and now into a fourth, Toyko. Nathan has delivered nutritional programs to optimize health and performance to many athletes over the years, including World, Olympic and European Medalists across a spectrum of Olympic Sports. Outside of Olympic Sports, Nathan has experience consulting to Professional teams in the English Premier League, PGA Golf, NBA, NHL and MLB through his role as the Lead Performance and Clinical Nutritionist and Scientist at the Sports science and data analytics company ORRECO. His research to date has focused on biomarkers, oxidative stress in elite endurance athletes, and unexplained under performance syndrome (Overtraining Syndrome). He has published in peer reviewed Sports Medicine and Science Journals and collaborated on various book chapters in the field of Sports Nutrition and Exercise Science.
Podcast Transcription
Hello and welcome to theSt Emlyns Podcast. I’m Simon Carly, and today we’re going to do something a little bit different, but very much related to the current COVID-19 stroke, coronavirus, stroke, SARS, COVID-2 outbreak. We’re getting together with a couple of experts in their fields to talk about aspects of well-being, support, immunology, nutrition, exercise, sleep, and a whole range of things which we think are really important as we think about how we are going to get ourselves and our colleagues through the next few months.
I’m going to start by getting them to introduce themselves. I’ve got two people on the podcast with us today, which is a bit unusual for us, so bear with us on the editing. Guys, do you want to introduce yourself? John, you go first.
Hi, Simon. I’m John Rogers. I’m a consultant in Sport and Exercise Medicine in Manchester. Over the last 12 to 14 years of my career, I’ve worked a lot with endurance athletes in British athletics and at British Triathlon. We see a lot of respiratory tract infections in the athletic population that we look after. It’s probably the biggest time loss factor, medical factor that we see. As a result of that, there’s been a lot of scientific intelligence and resources put into the prevention of respiratory tract infections during my career. I’ve worked with my colleague, Nathan Lewis, over the last 12 years, and we’ve seen a lot of athletes who have had problems with fatigue and overreaching because of the significant volumes and intensities of training and the stress, both physical and psychological, that comes with competing at major games and in very high-pressure situations.
Nathan?
Hi, Simon. Yes, I started out clinically and initially trained as a dietitian. When I left the NHS, I was working in intensive care, supporting athletes and prescribing nutrition to patients in that setting. I subsequently went on to do a PhD in Exploring Fatigue and Oxidative Stress in elite endurance athletes. I’ve worked for the English Institute of Sport as a nutrition scientist and as a nutritionist for the last 15 years across four Olympic cycles. I also work for a company called Orreco, which specializes in recovery solutions and biomarkers for elite athletes around the world. My day job now is very much focused on the elite athlete.
You guys are both experts in your fields. There’s no danger in us ever doubting the credibility here, and it’s fantastic to have people like you just so local. One of the things I’ve learned a little bit over the past few weeks with the COVID-19 outbreak is we’re breaking down walls, speaking to different people that we didn’t speak to before, and we’re learning huge amounts from each other. That’s kind of what I want to get out of today.
As we sit at the moment here in Manchester, we’re on the upswing of the curve of cases that are coming through, and we’re seeing some really quite terrifying stuff coming through the doors. We also have a workforce who are potentially facing one of the toughest times of their careers over the next few months. They’re stressed, anxious, and worried, but they’re also up for it. They’re ready, prepared, and they want to be as good as they possibly can be. We also need to flatten the two curves. I talked about this on one of the other podcasts. There’s a curve of general population infections. We need to flatten that to keep under NHS resources, but we also need to flatten the curve of healthcare worker infections. If we all go off sick at the same time, we’ve got a major problem because there will be nobody to look after the patients, who will be us. Anything that we can do to support our staff to stay healthy and recover quickly is really important. That’s why I’m really delighted that you guys have come along today.
We always take an evidence-based approach at St. Emlyn’s, and I know that you’ve got some ideas, thoughts, papers, and evidence to talk to us about today. Do you want us to kick off? Where do you want to start with how we can keep ourselves in tip-top condition during these difficult few months?
If I start, Nathan, with some of the background on lifestyle factors and then maybe you pick up on the nutritional side of things, is that okay?
Thanks, John. Yeah, great. I think the three big areas, Simon, for me were sleep, stress, and exercise. There’s been a lot of research in the sporting population around these areas. On a conference call on Friday with Nathan and various sports science people in North America and the UK, one of the presenters was Ricky Simpson, an exercise immunology researcher in Houston. Ricky’s research has focused a lot on exercise and the pros and cons of exercise on the immune system. He works with NASA and astronauts to optimize their immune health, and also with cancer patients and athletes. Some key papers on reducing respiratory tract infections and optimizing our innate and acquired immune response highlight the benefits of sleep. Professional sports have invested heavily in this area over the last three to five years, aiming for at least seven hours of sleep a night. The general advice is to look at sleep hygiene, minimize caffeine in the afternoon or evening due to its long half-life, reduce screen time in the evening as it can adversely affect sleep, and ensure your bedroom is dark, warm, and comfortable. Good quality sleep can have a really beneficial effect on your immune system.
In the months ahead for our frontline staff, the first rule is don’t become a casualty yourself. You’ve got to look after yourself. We don’t want people burning out. It’s a marathon, not a sprint. Try to look after yourself as well as you can and make sure you’re recovering and have downtime to avoid excessive stress.
Stress is another big area. We know stress is closely related to the immune system, affecting the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system. Managing stress appropriately can enhance immune health, but high stress levels, which are inevitable over the coming months, can increase your risk of infection. Think about strategies to minimize stress, like exercise or meditation. There are many good resources out there around mindfulness and different apps. I use an app called Calm, which I find very helpful for meditation.
Exercise has many beneficial effects on physical and psychological health. The general CMO guidelines for health and well-being recommend 150 minutes per week of moderate-intensity exercise or 75 minutes of higher-intensity exercise, along with strength training twice a week. While excessive exercise can stress the immune system, 30 to 60 minutes of exercise a day, five days a week, keeps you fit and healthy, helps you sleep better, and manages stress.
So, a couple of things I want to ask you about there, if that’s okay. There’s a great book called “Why We Sleep” by Matthew Walker, which we reviewed on the blog. It offers amazing advice about sleep, touching on many of the things you’ve mentioned. Of course, many of our workers work shifts, which disrupts sleep patterns, but there are ways to mitigate that.
Hospitals seem to run on caffeine, but there is good evidence that having caffeine in the hours before you sleep, particularly after lunchtime, can disrupt sleep patterns. Alcohol, another common crutch during stressful times, also disrupts sleep patterns. These are stresses that affect people due to the nature of our work, but they are changeable and adjustable.
Absolutely, Simon. I’ve read Matthew Walker’s book as well—a fantastic piece of work. He advises professional sports on sleep strategies. Caffeine has a long half-life of around 12 hours, and even decaffeinated coffee can contain about 30% caffeine, impacting sleep quality and quantity. Alcohol can help you get to sleep quickly but adversely affects sleep quality. Sleep is crucial for optimizing immune health, so it’s important to practice good sleep hygiene, especially given the challenges with shift work and trying to sleep during the day.
Couldn’t agree more. Quick solutions include sleep masks as alternatives to blackout curtains, ear defenders or ear plugs if you can tolerate them, and having a regular routine when you come home from a shift to help your body adjust. Reducing screen time before bed is crucial, although there’s some debate about the efficacy of removing blue light from screens.
These are all marginal gains that can significantly improve sleep and overall health. There’s a lot of focus on avoiding exposure to COVID-19 through PPE, isolation, and hand hygiene, which are all crucial. But we also need to support our own immune defense to cope with inevitable exposure.
Regarding mindfulness and yoga, there’s a free offer from 10% Happier for NHS workers, available for six months. Other apps like Headspace are also beneficial. My yoga teacher offers online classes now, which is a great way to stay engaged. Some might think of mindfulness and yoga as unconventional, but they are incredibly useful relaxation techniques.
Absolutely, Simon. In recent years, we’ve seen a lot of engagement in mindfulness and meditation within the athletic population. Headspace is a key app we use with athletes, and there’s been a growing focus on mental health due to competition stress and long-haul travel effects on sleep. We promote these tools among our athletes.
We’re not endorsing any specific app here, but these are examples of what’s available. There are free and paid versions of these resources, so find something that suits you.
Another important area is hydration and oral health, which are crucial for optimizing immune health. Athletes on long-haul flights are advised to stay well-hydrated and chew gum to increase saliva flow rates, improving mucosal health. Salivary IgA is a key part of oral immune health and can be relevant to initial exposure and defense.
Excellent tips, John. These are all achievable steps. Think about your routines and lifestyle, and see how you can make adjustments to improve your health and well-being.
Nathan, you’ve got a lot of expertise in nutrition. This is often a controversial area, but there is substantial evidence supporting the impact of nutrition on immune function. You sent me several papers, including Cochrane
reviews. Let’s delve into the nutritional side of things.
Absolutely, Simon. Sports nutrition and sports science have produced a wealth of evidence-based research. Looking at high-level evidence, such as meta-analyses and Cochrane reviews, we see significant findings related to nutrition and immune health.
Vitamin C, for example, has been well-researched. Linus Pauling’s work in the 1970s highlighted its benefits, and subsequent studies have supported this. A Cochrane review of five studies in heavy exercisers showed a 50% decrease in upper respiratory tract infections with vitamin C supplementation, typically around 250 milligrams to one gram per day. Achieving one gram a day through diet is challenging, but 200-250 milligrams is possible with a diet rich in fruits and vegetables.
Polyphenols, particularly flavonoids found in fruits, vegetables, tea, and coffee, also play a role in reducing upper respiratory tract infections. Meta-analyses show a 30% reduction in URTI incidence with flavonoid intake.
Research in athletes experiencing fatigue has shown lower levels of carotenoids in their blood, which are biomarkers for fruit and vegetable intake. Ensuring a diet rich in these nutrients is crucial. Aim for seven to ten servings of fruits and vegetables a day. If that’s difficult due to long shifts, consider soups, smoothies, or green powders to boost intake.
That’s fascinating, Nathan. The idea of testing blood for dietary intake is mind-blowing. Seven to ten servings of fruits and vegetables are higher than typical recommendations. What are your thoughts on supplements to achieve these levels?
Supplements can be helpful. Research in military personnel and stressed law students has shown benefits from green supplements, which contain dehydrated vegetables, herbs, and fruits. These can be added to recovery drinks or smoothies to boost intake of phytonutrients, which you won’t get from a multivitamin.
It’s important to mention vitamin C in the context of sepsis. Recent studies in critical care have shown it doesn’t have the expected effect on septic shock patients. However, in the context of prevention and reducing infection severity, vitamin C remains relevant.
Vitamin C deficiency increases the risk of respiratory infections and affects their severity and duration. Avoiding nutritional deficiencies is crucial for immune function. Ensuring adequate vitamin intake supports both innate and acquired immune systems.
Probiotics are another area with strong evidence. A Cochrane review of 12 studies showed a 50% decrease in upper respiratory illness incidence with probiotics. Probiotics can be consumed through drinks like Actimel and Yakult, which have shown favorable antibody responses to vaccinations.
Vitamin D is also vital. Many people in Northern climates are deficient, especially without supplementation or sun exposure during winter. Vitamin D supports immune function, influencing antimicrobial peptides in respiratory secretions. Supplementing with 2,000-4,000 IU of vitamin D3 daily is advisable if you haven’t been taking it during winter.
Omega-3 fatty acids, particularly EPA and DHA found in fish, play a crucial role in the inflammatory response and resolving inflammation. If you don’t eat fish, consider supplements to ensure adequate intake.
To summarize, we’re trying to apply evidence from one group (athletes) to another (healthcare workers) to optimize health during this pandemic. This is a reasonable approach given the physiological similarities and the current lack of specific research on COVID-19.
Thank you both for your insights. We’ll put notes on the blog, including links and references to the papers you mentioned. This information can help flatten the curve of healthcare worker infections and ensure we have enough people to treat patients. Thank you, John and Nathan.
References
- Recommendations to maintain immune health in athletes https://www.tandfonline.com/loi/tejs20
- Probiotics https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006895.pub3/epdf/full
- Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials https://pubmed.ncbi.nlm.nih.gov/23840373/
- Vitamin C for prevention and treatment of pneumonia https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013134/full
- Vitamin C and common cold https://www.cochrane.org/CD000980/ARI_vitamin-c-for-preventing-and-treating-the-common-cold
- Effect of Flavonoids on Upper Respiratory Tract Infections and Immune Function: A Systematic Review and Meta-Analysis https://pubmed.ncbi.nlm.nih.gov/27184276/
- Vitamin C and Infections https://pubmed.ncbi.nlm.nih.gov/28353648/
- Zinc lozenges and the common cold: a meta-analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage https://pubmed.ncbi.nlm.nih.gov/28515951/
- St Emlyn’s wellbeing resources https://www.stemlynsblog.org/tag/wellbeing/


Pingback: Hold deg frisk! Covid-19 og immunologi under koronakrisen – Luftambulanse forum
Pingback: Optimising your ability to Fight Infection - St Emlyn's High
Pingback: COVID19 kontroverser: PPE – probabilistisk fortalt, asymptomatisk spredning, sen intubation og opdaterede praktiske råd – Akutmedicineren.dk
Pingback: Stay healthy! Covid-19 and immunology in the time of corona – Airambulance forum