I’ll admit I was very excited and honored to receive the invite to speak in-person at the London Trauma Conference. I’d had the pleasure of speaking there in 2019, and that was my last international conference prior to the pandemic being declared. Following two years of primarily virtual conferences (with their inherent pros and cons), I was ready to challenged and educated by my fellow speakers. Clearly, the over 600 attendees felt the same way, and it was wonderful to see that hardly a seat was empty in the auditorium.
On my way back home to Philadelphia, I reflected on what makes LTC unique. It brings together some of the best minds in trauma care from only London, but nationally and internationally. Attendees and speakers came from as far away as New Zealand, injecting new energy and perspective into what we thought we knew about trauma care. It also provides a great forum for budding scientists with the always educationally amusing “Stand Up Science” session. And all this under the auspices of the impressive Royal Geographical Society.
Let’s run through the highlights from the first day of this conference.
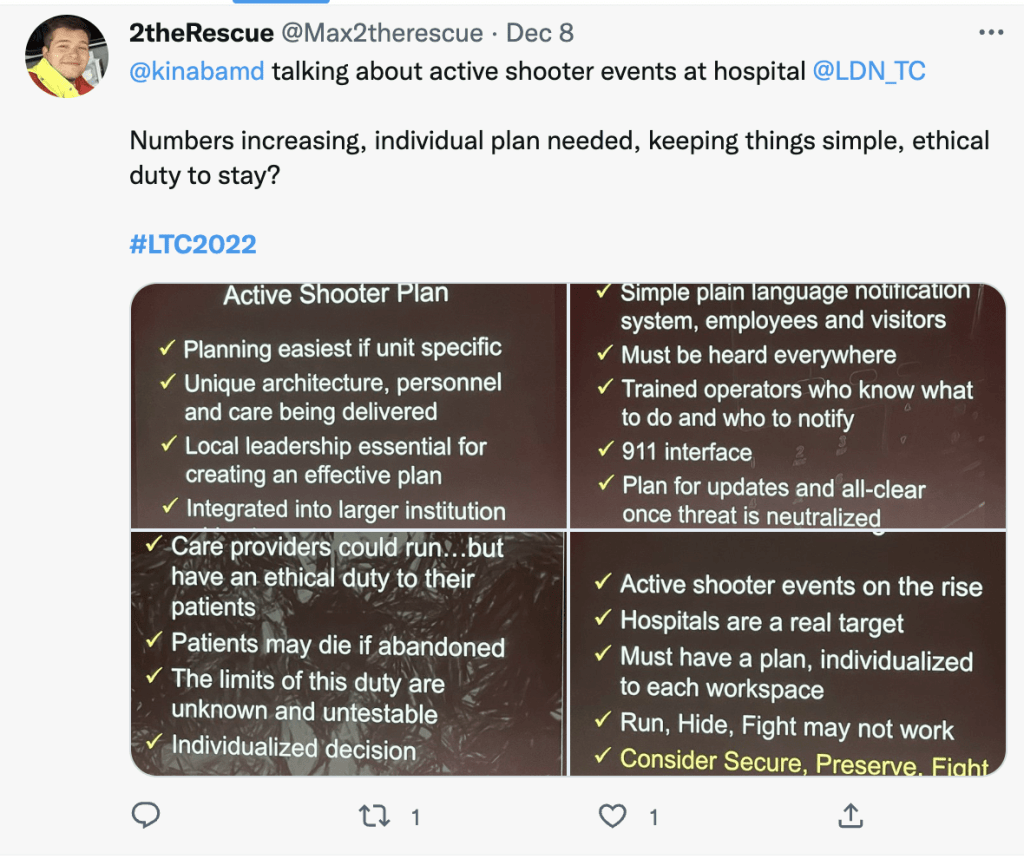
The first session covered major incidents. Kenji Inaba took the stage to discuss managing the active shooter who may end up at the hospital. Kenji can provide a unique perspective on this, as he is not only a trauma surgeon in an extremely busy level 1 trauma center, but is a serving police officer with the Los Angeles Police Department. While these are sadly more likely to occur in the US, the increasing violence worldwide means that a disgruntled patient, family member, or other individual may decide to exact their grievance upon the hospital and its staff. Having an individualized plan is key, and should incorporate a secure (the location), preserve (lives of patients and self), fight (only if necessary) approach rather than a run, hide, fight that has been recommended in other settings. A real ethical question is does your duty of care to your patients require you to stay with them or leave when faced with such a threat.
Principal physiologist Dr. Emrys Kirkman has a unique perspective on blast injuries given the work he does at the Defence Science and Technology Lab at Porton Down. With an ongoing threat from blasts (both criminal and otherwise), it is always worthwhile having a refresher on the effects of blast waves and projectiles set in motion by blasts that can lead to devastating injuries to various body organs.

This talk segued into a topic that is close to the St. Emlyns’ teams hearts – the Manchester Arena bombing. Sir John Saunders has just released volume two of a three-part report, and Dr. Phil Cowburn discussed the lessons to take away. As with many major incidents, communication failures were cited. What is clear is that care needs to be administered earlier, during the “care gap” that occurs from the incident to the arrival of professional services. This has been the aim of US courses like Stop the Bleed. Ultimately, this incident highlighted the need to overhaul outdated joint emergency response policies, and the lessons must be taken up or else the tragic deaths of 22 innocent civilians will have been for naught.

Rounding up this session was Dr. Marie-Louise Sharp on health and well-being in the emergency responder. We as a group are subject to immense trauma, compounded by the rigors of shift work. The PTSD, suicidality, and anxiety levels are significantly higher than returning soldiers, and yet our support systems are inadequate and underfunded.
Session two began with MedSTAR retrieval doctor Andrew Pearce talking about the trauma handover. This really needs to be the single point of truth, and being able to provide a succinct but thorough handover is essentially a procedural skill that requires training and education. This group has implemented video review to discuss areas of strength and improvement. Other systems can benefit from emulating their approach, so that we can improve upon the shocking statistic of as low as 36% of handover information being recalled by the trauma team.

The prehospital use of blood is a hot topic, and trauma and vascular surgeon Ross Davenport is ideally placed to run through the current literature. Are our stored blood products designed for trauma use (probably not), and what are we trying to achieve? Is it to pay back the oxygen debt, to repair the endotheliopathy, or prevent organ failure? When we study this, what end-point is truly meaningful for our trauma patients? Finally, is whole blood the answer? We don’t know the answers to these questions fully, but we seem to be on the right path. The upcoming SWIFT trial will hopefully provide some more answers.
Professor Karim Brohi provided his vision of the future of trauma research in LTC’s first keynote address. While we understand why early deaths happen, despite our advanced interventions we are still seeing late deaths, likely from cardiogenic shock as opposed to other organ systems. We need to focus on providing more tailored approaches by improving our knowledge and decision-making (lab tests to tell us what level of badness is happening, anyone?) and then to use this knowledge to guide prevention measures. More importantly, since trauma remains one of the leading causes of death worldwide, it deserves more funding as is afforded to cancer research. Great talk!

Mr. Peter Bates, consultant orthopedic surgeon, provided a funny talk on their role in the trauma team. Yes, part of it is hitting things with a hammer, but the crux of their job is to enable rapid mobilization to promote recovery. Immobility leads to a world of problems in all age groups. Coordinating with the team to provide damage-control orthopedics at the right time (and with the right hammer) can be critical to overall care.

Perhaps the highlight of the conference for me was to hear and meet Sir David Nott. If you haven’t yet read his book, please do. He described in an incredibly self-effacing manner his incredible contributions to the worldwide education of combat surgery. What particularly struck me was his rapid evolution of teaching style and delivery to meet the needs of those who needed it most – when a course in the UK wouldn’t work, he brought the course to the people, creating a versatile mannequin to help with the training. Incredible to see him and his work recognized in many ways, including one of several faces on this year’s cover of Time Magazine Person of the Year. “Be nice, kind, and remember the patient…”

Quick coffee break then onto Dr. Sabrina Cohen-Hatton, a psychologist and Chief Fire Officer for West Sussex Fire and Rescue. She delved into the psychology of decision-making under pressure, something we may face on an almost daily basis. Uncertainty increases stress, which increased the tendency to rely on rules even when they did not exist for that situation. She reviewed the use of pre-action checks to improve situational awareness, asking why am I doing this, what do I expect to happen, and what is the benefit versus risk.
I was next up on stage discussing the ED management of gunshot wounds. Although this is certainly a very prevalent American problem, just in the days since I’ve returned from LTC I’ve seen headlines of shootings in Rome and Australia. Although other countries will thankfully see less of this than the US, it is vital that when you do have a patient who has had a gunshot wound that you acutely focus on what may be an uncommon presentation. Some key points are that velocity matters more than caliber, it is critical to identify injury points early by thoroughly examining the patient on arrival (including axillae and groins), and to obtain cavitary triage through plain x-ray imaging as bullets can really end up anywhere. Finally, not all gunshot wounds need the operating room – but this approach requires careful selection and protocolized care.

My friend Mike Abernethy rounded out LTC Day 1 with a fascinating talk on farm-related trauma. These injuries truly have no respect for geography, politics, or physiology. Farm equipment injuries far outweigh animal-related injuries, but both can be devastating. Children are particularly vulnerable in this arena, and Mike recounted a fantastic effort by his MedFlight HEMS colleagues in saving a young boy’s life. It’s worth keeping in mind that folk who live on family farms are much harder to kill than ordinary people, but they will try much harder.

That was day one of this fantastic conference. The conversations continued in and around Kensington over good food and drink. I’ll bring the highlights from Day 2 in my next post.
Take care,
Zaf
@ResusOne

