When I trained here in Virchester we had a fairly aggressive approach to the management of pneumothoraces. All trauma pneumothoraces got chest drains, a chest drain meant an open one, the size was as big as possible and the analgesia was homeopathic. Looking back those were not great times for the patient, but because of the procedure paradox we did learn a lot, and arguably ‘looked forward’ to the procedures.1 In stark contrast, the patients clearly did not.
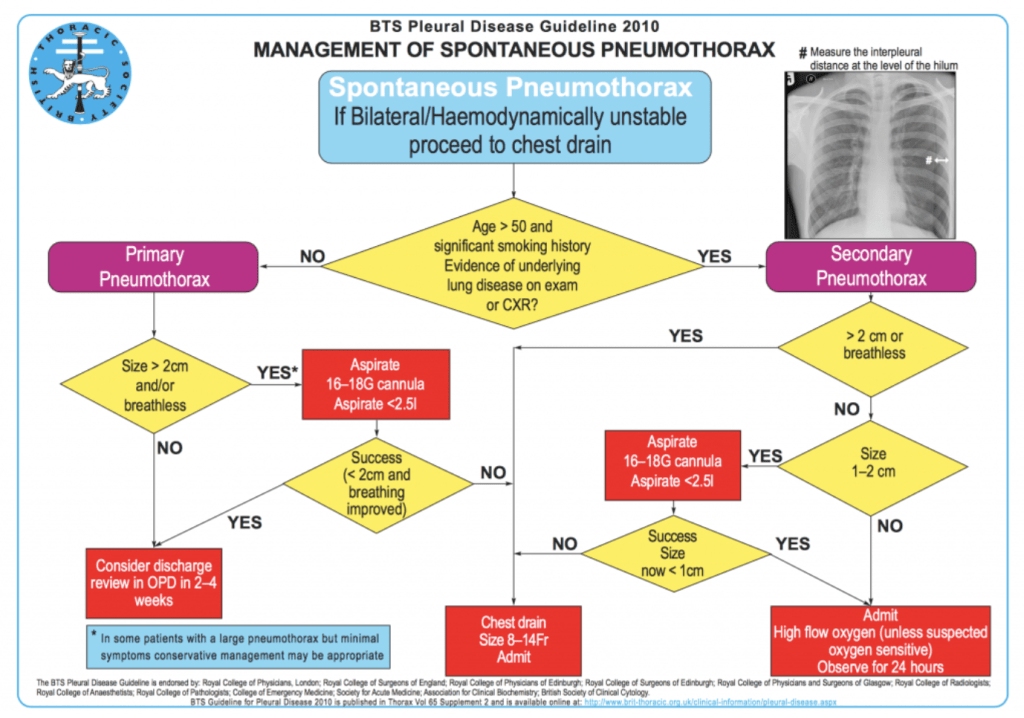
We’ve blogged in the past on the increasingly conservative management of traumatic pneumothoraces2, and in our current practice this is what we do. Small and asymptomatic traumatic pneumothoraces are now managed conservatively in our practice, but what about the patients who present with the ‘medical’ pneumothoraces? For them little has changed as we still follow the BTS guidelines3 which recommend aspiration and/or chest drains for moderate, large, secondary and symptomatic pneumothoraces. The BTS guideline is shown below.
American guidance is even more aggressive, with an approach to just go for chest drainage4.
The bottom line is that we do put quite a lot of chest drains in for medical pneumothoraces. Almost always this means a small (12F) Seldinger technique which is great for patients, but it does need an admission and quite a lot of faffing about. This of course is in contrast to the direction of travel in the management of some of our traumatic pneumothoraces. Could we be more conservative in that group as well? A recent systematic review noted that the evidence to support decision making in this situation is poor5.
This month we have a paper in the NEJM6 that may help answer that question. It’s received quite a bit of interest in the #FOAMed world already, but as it’s directly relevant to our day to day practice it’s worth a look from the St Emlyn’s team.
You can read the abstract of the NEJM paper6 below, but as we always say PLEASE read the full paper yourself and make up your own mind before changing practice.


What kind of paper is this?
This is a randomised controlled trial which is the appropriate design for an intervention, or as in this case, the lack of an intervention. This is a non-inferiority trial in. that they were trying to find out whether conservative management was non-inferior./no worse than interventions. The margin of non-inferiority that they chose was 9 percentage points. In my opinion that’s a pretty big margin (Ed – close to an NNH of 10). Clinically I would have hoped for a much smaller non-inferiority margin than one in 10 patients.
Tell me about the patients.
These were patients with spontaneous and pretty large pneumothoraces, certainly of a size that we would currently try and drain here in Virchester. Patients aged 14-50 with a pneumothorax of >32% were eligible7. Patients were recruited in 39 Antipodean emergency departments.
What did they do?
Very simply, patients were randomised to either a conservative watch and wait approach. They had another CXR at 4 hours and if that was OK, the patient was well and not distressed then they were allowed home. Many patients needed more than 4 hours of chest drain placement, but it could be removed after a minimum of 4 hours.
The intervention group had a 12F Seldinger drain just as we normally do here in Virchester. However, in this study the drain could be removed as early as 4 hours. That’s a lot sooner than we remove them here in Virchester which may be an important difference between this study and our practice.
Patients were followed up at 24 and 72 hours and then again at 2, 4, and 8 weeks.
What were the main results?
They recruited 316 patients over a 6 year period. Of the 316 patients who entered the trial 272 made it through to having had a follow up CXR at 8 weeks. In other words the drop out rate was quite high, although they had taken some account of this in their sample size calculations where a significant drop out rate had been anticipated. However, we don’t know the outcomes for those missing patients.
In terms of the primary outcome, when excluded missing patients 98.5% of the intervention group had resolved their pneumothorax in comparison to 94.4% in the conservative management group. That’s a risk difference of −4.1 percentage points; 95% confidence interval [CI], −8.6 to 0.5; P=0.02 for
non-inferiority. So in the opinion of the authors non-inferiority has not been demonstrated. However, as we mentioned above it’s quite a large inferiority margin.
In the secondary outcomes there was again a trend towards benefits to a conservative approach. Fewer days off work, fewer interventions and a lower recurrence rate as examples. These may well influence your decsion as to whether to offer conservative management. The reason for a lower recurrence rate is interesting as I can’t think of a pathophysiological mechanism for this.
Notably, no patients in the conservative management group required emergency intervention, so within this relatively small group of patients in the trial it was safe. However, this trial is too small to assure us of the safety of this approach if applied in practice.
What does this mean for our patients in Virchester?
I was hopeful that this paper would convince me that a conservative approach is the way to go, but this paper has some concerns. The drop out rate, a number of protocol violations, the large inferiority margins and the short intervention time for some patients means that I don’t think it directly answers or questions our practice in Virchester.
I’m also intrigued that it took 6 years across 39 centres to recruit this number of patients. That seems a long time across a very large service. The number of patients screened was over 2600 suggesting that this data only applies to a very small subset of patients with spontaneous pneumothoraces.
That, together with the relatively low level of intervention required by a 12F Seldinger technique, means that I think our practice will largely remain the same. However, in some patients, perhaps those who aren’t very keen to have a procedure done I do now know that a conservative approach appears to be a reasonable and probably(?) safe option. The accompanying editorial in the NEJM comes to roughly the same conclusion, similarly describing the analysis as ‘statistically fragile’.
The summary from NEJM in video is a more positive as shown below.
Update: The authors of the paper are much more positive about their own findings and I would encourage you to read their rebuttal in the comments section below. I think the question they are challenging us with is, ‘what would make you change practice, if not this paper?’. That’s a fair question (it was one of my SMACC talks in fact), and I think the answer is complicated. Offline I’ve had some great chats with Gerben Keijzers, some of which you can read in the comments section below. It’s always really interesting to hear the insider view of a trial as there is always more clarity available than from the print version in the journal.
What is very interesting is the experience post trial where they have adopted a more conservative approach, apparently with success. That data is not yet published, but should it be, then that would be very influential in changing practice.
The bottom line
Conservative management of moderate and large spontaneous pneumothoraces is an option, but we will wait for changes to the BTS guidelines before changing our regular practice.
vb
S
References
- 1.Carley S. DFTB. The procedure paradox update. St Emlyn’s. https://www.stemlynsblog.org/how-it-felt-the-procedure-paradox-update-dftb/. Published 2020. Accessed 2020.
- 2.Carley S. Conservative management of chest trauma. St Emlyn’s. https://www.stemlynsblog.org/jc-conservative-management-of-chest-trauma-st-emlyns/. Published 2018. Accessed 2020.
- 3.MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax. August 2010:ii18-ii31. doi:10.1136/thx.2010.136986
- 4.Baumann MH, Strange C, Heffner JE, et al. Management of Spontaneous Pneumothorax. Chest. February 2001:590-602. doi:10.1378/chest.119.2.590
- 5.Ashby M, Haug G, Mulcahy P, Ogden KJ, Jensen O, Walters JA. Conservative versus interventional management for primary spontaneous pneumothorax in adults. Cochrane Database of Systematic Reviews. December 2014. doi:10.1002/14651858.cd010565.pub2
- 6.Brown SGA, Ball EL, Perrin K, et al. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. N Engl J Med. January 2020:405-415. doi:10.1056/nejmoa1910775
- 7.Collins CD, Lopez A, Mathie A, Wood V, Jackson JE, Roddie ME. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. American Journal of Roentgenology. November 1995:1127-1130. doi:10.2214/ajr.165.5.7572489


Thanks for your analysis Simon, St Emlyns can always be relied upon to keep us up to date! A really interesting paper for me – because both treatment arms represent an evolution in practice for me and my department. I would love to be able to send these patients home as per the protocol for the observation arm, but I think even the intervention arm represents a positive change in practice. Whipping the chest drain out at 4 hours is more aggressive than I am used to, but I think this study supports the safety of this approach. Of course, all of this relies on having access to early follow up.
While I agree that the changes in outcomes between the two arms are “statistically fragile” (as the authors themselves point out), both approaches appear safe, and I am certainly going to start these conversations with our respiratory colleagues.
Great to hear from you again Gareth. I’ll be really interested to hear how those conversations go on.
Thanks for appraising this paper.
Some counter commentary to the points made
The non-inferiority margin of -9% is deemed large and this is translated to a NNH of ten. It would be interesting to ask clinicians and patients if they think that a small persistent apical pneumothorax at week 8 truly represents ‘harm’.
Another way to look at this non-inferior margin is to ask (the patient): “If we put a drain in, we are 99% certain your x-ray will look normal in 8 weeks. If we do nothing, the chance of a normal x-ray may be lower, but it would definitely require an intervention with inherent risks and a hospital stay of a few days. What would be an acceptable chance of a normal x-ray for you to attempt conservative treatment?”.
Based on such an approach a non-inferiority border of 90% is likely reasonable for a most patients and clinicians (Some people may be happy with 70 or 80%, they can always have an intervention down the track – no need to rush).
As such the NNH argument needs to be put in context against the real harm from a drain (NNH ~ 5)
With regards to the missing data, indeed some patients did not present for their 8-week x-ray. We could usually phone them and establish that they were fine (We knew they were still alive), but to get them back for an x-ray was tricky at times (likely a result of the demographic). The conservative group had higher drop-out rates which was simply because they were fine and did not worry (based on my experience as a recruiter of >20 patients in this study)
The last comment to address is the issue of generalisability. Indeed 2600 patients were screened, where less than 20% if those were included. Mostly this relates to the fact that this is an unblinded study. The patient is provided with 2 options: a) we can put in a drain and this is guideline based, or b) we can just observe to avoid unnecessary intervention because we think it may be just as good.
It is often difficult to convince the patient (and treating doctor) about the clinical equipoise, so many patients who were eligible declined to consent as they preferred one treatment over the other. The declining patients had similar demographics, synptoms and pneumothorax size, and as such it is likely that these findings also apply to the non-consenting group of patients.
Now here is the interesting part, over the first few years of the recruitment period, about 80% of eligible patients declined consent in my centre and most ended up with a drain outside the study (as part of routine guideline-based management). However, in the last few years of the study, still 80% declined consent, but now most chose conservative management. This is likely due to treating clinicians’ changing their belief about equipoise after seeing our experience with conservative treatment. Our most recent audit shows that in the last year (after the study finished recruitment) 95% of PSP was managed conservatively with no serious adverse events.
These are all interesting explanations/interpretations of the results. I might cheekily suggest that they are not entirely unbiased though. For example you presume that the conservative group had a higher drop out rate because they were ‘fine’. That of course may well be the case, but it is a presumption and not a fact.
The question about what patients would believe to be a reasonable non-inferiority margin is truly an interesting one. However, I don’t think that was asked or studied in this paper. If it was I could not find it.
Similarly, the reasons for not taking part in the trial are a presumption. I cannot see the data in the study that tells me why patients decided not to take part in the way that you describe.
Lastly the audit you state at the end does not state what type of patients were managed conservatively. If that includes the small PTXs that we have always managed conservatively then it might exaggerate the success rates. It also asks the question of numbers because only 20% of patients in the original trial were included, this suggests either a consent issue was preventing people in the past OR the range of patients now offered conservative management is outwith the inclusion/exclusion critieria of the original trial. Obviously I cannot know which as I don’t have your audit data, but a 20% in trial to 95% in practice is an interesting and dramatic change in practice.
So, in summary I can absolutely see where you are coming from on this. You have experience of the trial ‘from within’ whereas we are just looking at what is published and there are always differential interpretations because of that. I think your current cohort of conservatively managed patients will be fascinating to follow up and indeed potentially publish to show if the paper has changed clinical practice safely and positively. I suspect it may well do this.
Thanks for the comments. I think this paper may well change practice, but I’m remaining a little sceptical for the moment until we are little clearer regarding patient mix, follow up, observational support for the conservative strategy. In large part because the 4 hours and then remove strategy is not something we do here. In that regard the intervention tested in this trial would also be a change from our current practice.
What’s important to us is that people read the full paper themselves (it’s a good paper and study) and come to their own conclusions. Have a great weekend 🙂
Pingback: Quiz 62, February 14th 2020
Dear Simon
Firstly full disclosure I was an author on the paper and I acknowledge my bias.
Thanks you for review of our paper, while I acknowledge some of the methodological and statistical concerns you have raised I would like you to reconsider their ‘clinical significants’ and reconsider the “Virchester way”
Current practise in the treatment of PSP is driven by guidelines based upon low-level evidence and opinion driven by physiological reasoning. As the accompanying editorial and Cochrane systematic review points out.
If you enjoy reading papers that challenge paradigm I would encourage you to read this fascinating paper from Thorax in 1966 by Stradling and Poole DOI:10.1136/thx.21.2.145 They question the new trend of inserting ICC for both primary and secondary pneumothorax based upon the belief that “recovery would be quicker and fewer relapses.”
This was their conclusion: “it is clear that the general policy of non-intervention and out-patient management for spontaneous pneumothorax has been fully justified. It can be recommended with confidence for the simple form and will be over 80% successful”
It’s a case of “Back to the future” and similar to the editorial summary of our paper: “We have learned much from this trial. Almost 85% of the patients in the conservative-management group did not undergo any intervention.”
Your comment that the editorial suggested the trial was “fragile” risks misleading your readers by taking them out of context and some people may confuse it as a reference to the fragility index. The full comment from the editorial is “the statistical evidence is described as “fragile,” but the basic point is that the conservative-management group did well.” I don’t believe it is a accurate description to suggest that the editorial came to same conclusion as your review. “On the basis of this randomized trial and the earlier reports, we should now be prepared to offer this conservative approach to the young, healthy person with a large primary spontaneous pneumothorax if there is no hemodynamic compromise.”
You are clearly right to question the drop out rate but I would argue it is a symptom of the patient group, young and otherwise well and the disease that is benign and self-limiting. Given Figure S5 in the supplementary papers demonstrate that independent of treatment arm everybody got better by 10 weeks that remain in the study I would ask what is your clinical concern about the patients that dropped out?
Also for your information as reported in paper in the intervention arm 78 or the patients had an ICC in place for more that 72 hours. ICC where only removed after 4 hours if the lung was fully inflated without evidence of air leak, so it may be more like the Virchester way than you suggested.
I am very concern and a bit perplexed that your review didn’t report any of the patient centred secondary outcomes. Adverse events where three times more common and recurrence at one year twice the rate in the intervention group. In fact as your reader can see from table 3 all the adverse in the study apart from a handful where the result of ICC insertion. I think that these factors as well as day in hospital and days off work will be of interest to your patients as well as your readers.
Our paper I believe mounts a strong argument for using shared clinically decision-making with your patients and setting up systems in you health service where the large majority of these patients can be treated with deliberate clinical inertia in the first instance.
Best Wishes and Hello from the Antipodean Diana
P.S.
Regarding your concern about high “protocol violation” (which I must say make me feel a little unclean) This is in fact not accurate. The protocol was explicit and reported as such in that patients care was only protocoled for the period of observation in the conservative arm and until decision to either remove ICC or reopen and continue inpatient management (typically 6-12 hours). After that time clinicians where free to manage the PSP as per there local guidelines. The true protocol violations where the 10 patient who consent then once randomised and the scalpel was opened they requested to be moved to the conservative arm. Many researchers may have been tempted to analysis that cohort as part of the conservative group (per protocol approach), as it would have made our results more impressive, but we choose the intention to treat approach.
It was always expected that a proportion of our cohort with go on the receive an ICC similar to what Stradling and Poole found.
Thanks for those helpful clarifications.
S
Thanks Simon and thank you for your update. This is what I love about #foamED
D
Pingback: Conservative treatment for primary spontaneous pneumothorax - First10EM
Pingback: Papers of March 2020 – The Resus Room
Pingback: Spontaneous Pneumothorax: Stand There and Do Nothing? - REBEL EM - Emergency Medicine Blog
Pingback: February podcast round up and thoughts on Covid-19. St Emlyn's • St Emlyn's
Pingback: EM Quick Hits 18 Conservative Management Pneumothorax, Microdosing Buprenorphine, Practical Use of CRITOE, Canadian TIA Score, Pediatric Surviving Sepsis Guidelines, Safety of Peripheral Vasopressors - Emergency Medicine Cases