This month the BMJ has published a trial on the use of convalescent plasma in the treatment of admitted patients with COVID-19 (the PLACID trial). Convalescent plasma therapy basically takes plasma, together with antibodies from patients who have recovered from COVID-19 and then transfuses that into patients in the acute phase of their disease. The idea is that the antibodies in the plasma will bind to any virus in the recipient and thus reduce the severity of the disease. It’s a therapy that has had many proponents and it’s been given to over 100,000 patients in the USA alone, but the evidence for its effectiveness in preventing death or severe disease is far from conclusive.
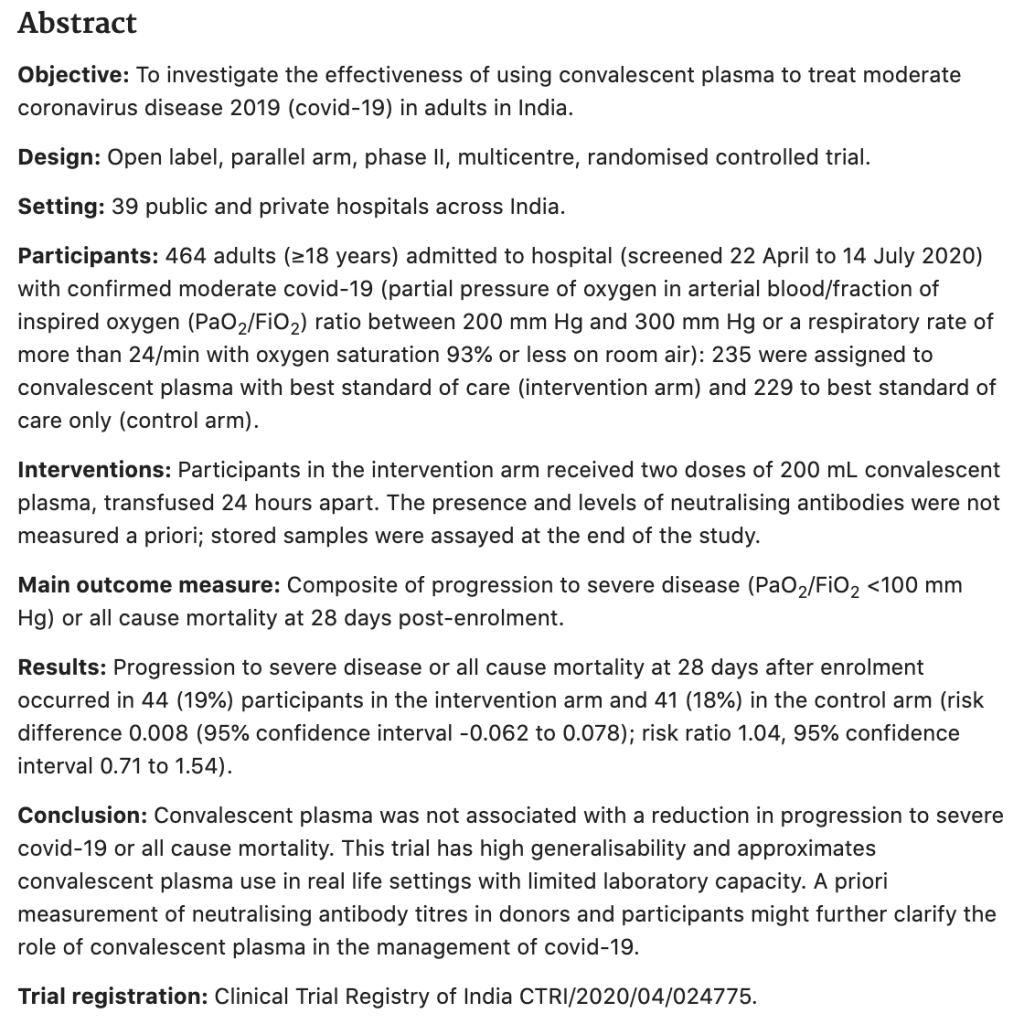
The abstract of the paper is shown below, but as always we strongly recommend you read the full paper online, especially as it is open access.
What type of study is this?
It’s an open label randomised controlled trial with randomisation being achieved using a stratified block randomisation strategy to allocate participants in a 1:1 ratio between convalescent plasma as well as the best
standard of care (intervention arm) or best standard of care alone (control arm).
As multiple sites and normal standards of care were used in this trial they stratified by site using block randomisation. This is a technique that is designed to ensure that there are roughly equal numbers of patients in each arm of the trial at each site.
This an open-label trial such that everyone would be aware of which treatment was given to patients. This is not gold standard (which would be blinding) and so that may introduce bias.
Tell me about the patients.
The authors recruited patients at 39 different hospitals across India. Patients had to be moderately unwell to get into the trial and thus were exactly the group that I worry about progressing to serious disease or death from COVID-19. Specifically they had to have either a partial pressure of oxygen in arterial blood/fraction of inspired oxygen ratio between 200 mm Hg and 300 mm Hg or a respiratory rate of more than 24/min with oxygen saturation (SpO2) 93% or less on room air. The patients look to be pretty similar at baseline between the groups.
What about the interventions?
The intervention group received 2 doses of convalescent plasma 24 hours apart. In addition all patients received the usual standard of care, which was quite variable. Patients received what was thought to be the best care by local clinicians at the time, and so patients also received many therapies that we now know are ineffective or perhaps even harmful (e.g. 68% of patients received hydroxychloroquine). That is an issue of course, but it reflects a pragmatic approach in a rapidly changing disease. Whilst a reasonable approach it does raise the question of compounding co-treatments when we look at the result.
What about the outcomes?
The main outcome in the trial was death or progression to serious disease defined as (PaO2 /FiO2 ratio <100 mm Hg) within 28 days. This seems reasonable as an outcome that is important to patients and clinicians.
What did they find?
The recruited a total of 464 patients between April and July 2020. The headline figure is that there was no difference in the primary outcome between the two groups, 18% vs. 19% (risk ratio 1.04, 95% CI 0.71-1.54).
For mortality the difference was 14% vs. 15%, so again no difference between the groups.
It was a similar picture for all the other secondary outcomes such as length of stay. No difference across the board.
The only ‘positive’ outcome of interest was a clearing of the virus by 7 days in the intervention group.
So what does this mean?
This trial suggests no benefit to patients from convalescent plasma which is a useful outcome. It is important to remember that this is still a relatively small trial conducted amongst patients with a standard of care that is very different to that which we deliver in the UK. There are other larger trials currently in progress, notably the UK RECOVERY trial, which are still randomising to convalescent plasma, and with a more consistent standard of care arm. It will be interesting to see whether these trials deliver a consistent message to the PLACID trial.
There was certainly lots of hope for convalescent plasma and this trial may be seen as a disappointment, but that’s science, and all data such as this is welcome if it helps us focus on therapies that might work. For the moment it would seem wise to only prescribe convalescent plasma as part of a trial and not as a routine therapy.
So why might it not work?
There is a very good commentary in the journal that makes suggestions as to why a negative result was found here despite evidence of a reduction in viral load at 7 days. That reduction suggests that convalescent plasma IS doing what we want it to do, that is finding, binding and destroying virus in patients. It’s just that this does not translate to a patient orientated benefit.
In the BMJ commentary the question of convalescent plasma being pro-thrombotic in a disease that we already know to be pro-thrombotic is a concern, although that was not tested in this trial. It is possible therefore that convalescent plasma may increase this effect (though this is supposition and not demonstrated in the trial).
Similarly we don’t really know the quality or quantity of antibodies in the plasma, the trial is not blinded and there was a lack of standardisation for some secondary outcomes. These may also affect the validity of the results.
As pointed out by @peterhoby below, there are also concerns that the plasma given to patients did not have high levels of antibodies. Roughly a third had no antibodies at all and many of the others had low titres.
My personal view is that convalescent plasma may be targeting the wrong phase of the COVID-19 disease. It’s a therapy that is intended to reduce the amount of active virus in the body, but it may not be that level that is responsible for the pneumonitis and other COVID-19 features that appear roughly 10 days after the initial infection. That latter process appears to be immune-mediated in a patient sensitised during their initial viraemia. We simply do not know whether the severity of this latter immune phase of disease (and the reason why most people die of the disease) is directly related to the amount of active virus in the early stages, but it seems unlikely to be the case. If so, the reduction of active virus may have no impact on the proportion of patients developing the later phases of disease. It’s worth reminding ourselves that the only proven therapy in COVID-19 affecting death or severe disease is steroid treatment which should have little or no effect on viral load, but it does have significant immuno-modulatory effects.
This study is consistent with the ConCOVID trial from the Netherlands that also showed no benefit from convalescent plasma. Similarly, the latest Cochrane review concluded that convalescent plasma therapy is unproven. This trial will not change that conclusion.
Final thoughts.
This trial is another great example of why we need high quality evidence in this pandemic. The fact that over 100,000 patients have been treated with a therapy that has not been shown to be effective in high quality trials is something that should worry us all. Just imagine how much more we would know about COVID-19 if less than 0.5% of those patients had been enrolled into a clinical trial?
We await the results of larger trials, such as RECOVERY to see if the evidence changes with more patients and more standardised care.
The bottom line is that convalescent plasma should only be recommended as part of a robust clinical trial that addresses some of the limitations of the PLACID trial.
vb
Simon
@EMManchester
- Estcourt LJ, Roberts DJ. Convalescent plasma for covid-19. BMJ 2020;370:m3516. doi: 10.1136/bmj.m3516 pmid: 32933945
- Convalescent plasma in the management of moderate covid-19 in adults in India: open label phase II multicentre randomised controlled trial (PLACID Trial) https://www.bmj.com/content/371/bmj.m3939
- ConCOVID trial https://www.medrxiv.org/content/10.1101/2020.07.01.20139857v1
- Convalescent plasma is ineffective for covid-19 https://www.bmj.com/content/371/bmj.m4072
- Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: a rapid review https://pubmed.ncbi.nlm.nih.gov/32406927/
- RECOVERY trial https://www.recoverytrial.net/

