Resuscitative thoracotomy remains a controversial procedure in prehospital and emergency care. This month we have more evidence of its effectiveness in prehospital care.
Despite significant advances in trauma care, we are still challenged with moving the needle in trauma mortality in those patients suffering profound hemorrhagic shock. Marsden and Harvin both showed the mortality in patients requiring an emergent trauma laparotomy, often for non-compressible torso hemorrhage, remains very similar over the last few decades – on either side of the Atlantic.
A significant focus of my recent academic work has been working with military and civilian agencies in pushing trauma critical care interventions closer to the point of injury – within systems that can support this. The aim is to address hemorrhagic shock at a point before it becomes irreversible. The earlier use of tourniquets, blood products, and even (much to the chagrin of some of my US friends) TXA have shown documented benefit.
Unfortunately, some patients succumb to the severity of their injuries and arrest, necessitating a resuscitative thoracotomy (RT). The literature is awash with papers looking at indications, contraindications, outcomes, and comparing RT for blunt versus penetrating trauma – sometimes with conflicting results. What does seem almost uniformly apparent, however, is that you’re more likely to have a better outcome the sooner it is done (like at the point of injury!). This is what piqued my interest in this recent paper from the Essex and Herts Air Ambulance Trust (EHAAT), published in the Scandinavian Journal of Trauma, Resuscitation, and Emergency Medicine.
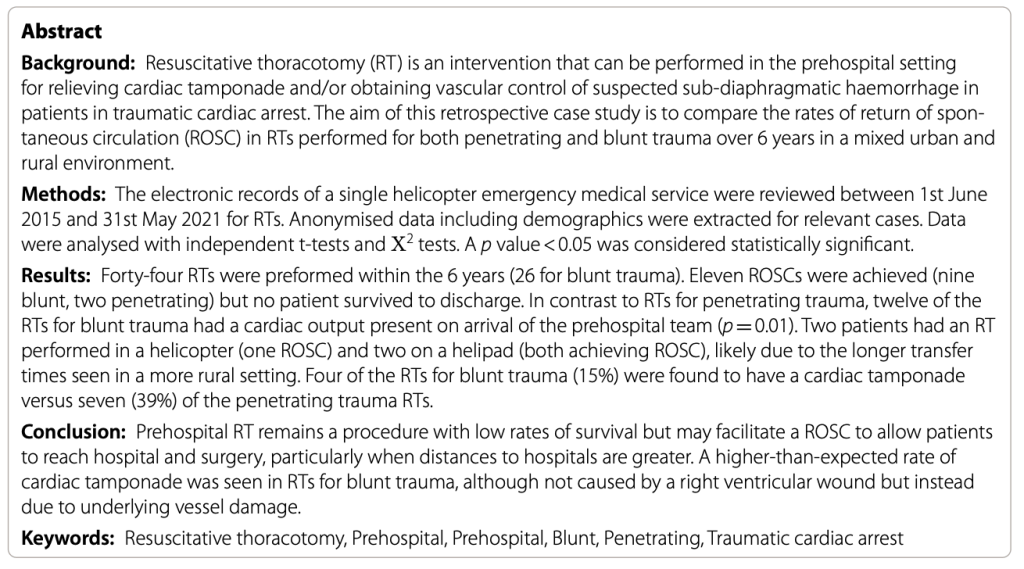
Here’s the abstract – as always, we advise you read the paper in full and come to your own conclusions.
What’s the clinical question?
Similar to many HEMS services in the UK, EHAAT is a physician/paramedic model that, along with 2 other HEMS services, covers a large urban and rural environment of around 6 million people spread over about 19,000 square kilometers. The service responds to scene primarily by helicopter during daylight hours, and a fast-response vehicle at night. All EHAAT clinicians undergo regular training and follow a standardized procedure to deliver a resuscitative thoracotomy when indicated. They list these indications as:
- A patient in cardiac arrest or in extremis, with penetrating injury to the chest, abdomen, neck, axilla or groin.
- Penetrating limb injury causing cardiac arrest, where immediate control of bleeding and vascular access cannot be achieved.
- Cardiac arrest following blunt trauma, where there were recent signs of life, absence of catastrophic head injury (based on history or clinical examination) and where it is felt that a treatable chest injury is the primary cause of arrest.
This paper outlines EHAAT’s outcomes for resuscitative thoracotomy performed for both penetrating and blunt trauma in urban and rural settings.
How was the data put together?
The authors retrospectively reviewed computerized medical records of their service over a 6-year period (2015-2021). They specifically looked at demographic data; dispatch, scene, and transport times; cause of injuries; presence or absence of cardiac output on arrival of medical services; and outcomes. Outcomes between penetrating and blunt trauma cases were compared.
Of note, this service introduced prehospital blood in 2019 (they carry 2-3 units of packed red blood cells and 4 units of lyophilized plasma). Therefore, they also compared outcomes before and after blood products became available.
What were the reported findings?
In the 6-year study period, 44 resuscitative thoracotomies were performed, for an average of 7.3 per year. The majority of the incidents and interventions occurred between 7AM and midnight, though recall the EHAAT team is available 24 hours a day. Ages ranged from 10 years to 85 years: the majority of the patients were males in the 20-40-year range. 58% were undertaken for a blunt injury mechanism, and the primary indication was either relief of tamponade or for aortic compression in the presence of a subdiaphragmatic injury. 38 resuscitative thoracotomyies were done at scene (3 were done in a vehicle, 2 on the helipad, and one in the ED at the request of the trauma team). Although 11 patients achieved return of spontaneous circulation (ROSC), unfortunately there were no survivors to hospital discharge.
When comparing blunt to penetrating mechanisms, the patients seemed well-matched in terms of age, sex, and mean response times. 18 and 12 of the blunt trauma patients had a cardiac output on arrival of the initial paramedic and subsequently the HEMS team respectively, compared to 8 and 2 respectively for the penetrating group. The relief of tamponade was the primary reason for the penetrating trauma resuscitative thoracotomy whereas there seemed an even distribution of need for relief of tamponade and/or aortic control in the blunt group. Although more penetrating trauma patients actually had tamponade at time of RT, a higher proportion of blunt trauma patients had both cardiac movement seen at RT as well as achievement of ROSC as compared to the penetrating group. Thus, a higher proportion of blunt trauma victims were transported to the hospital.
What are the systems details?
If you know me, you know I’m very much about systems of care delivery. Prehospital resuscitative thoracotomy won’t work (and shouldn’t be done) unless the whole system is in place to support this intervention. The authors do lay out in detail numerous aspects of their system-level approach here, from training to the ability to track various times along the patient journey. Importantly, they followed up not only patient outcomes in hospital but also, when available, post-mortem information. I have participated in military calls discussing mortalities which included input from the forensic pathologist/coroner. I think this information is invaluable in informing our approach to interventions and for continued professional development individually and as a service. As here, this should be incorporated into any similar civilian review.
For resuscitative thoracotomy to work, you must get to the patient in a timely fashion. The authors report mean times from 999 call to HEMS arrival of 29.9 minutes. Note with the large geographic area covered, the range of road times to the trauma center were 19-83 minutes (mean about 50 minutes). 11 of the 44 resuscitative thoracotomy patients were transported by ground, and 5 by air.
Following the introduction of blood products in 2019, a further 15 RTs were done, with 11 receiving blood products (about an even mix of blunt and penetrating cases). Only one was transported to hospital, none achieved ROSC, and the majority were pronounced dead at scene – an appropriate use of resources as all major resuscitation interventions could be provided prehospital.
What does this all mean?
First and foremost, hats off to the EHAAT team for candidly publishing their experience, even though sadly none of their patients ended up surviving. They clearly demonstrate that they can safely and appropriately deliver this intervention within their well-governed clinical system. To still publish essentially negative data actually reflects positively on their work ethic as an organization. The information does add to our overall understanding on this topic and can ultimately be used to improve trauma care.
Both patient selection and timing are important aspects. Patient selection can be challenging in a dynamic situation, and really is reliant on an experienced clinician making a rapid evaluation and judgment call. Clinical suspicion is often relied on, but ultimately only 15% of blunt and about a third of penetrating trauma patients in this cohort had a tamponade. Although aortic control was the defined reason in a significant portion of blunt trauma patients, this could potentially be achieved by other means (e.g. the abdominal aortic junctional tourniquet or even REBOA if available) than having to open the chest. Having ultrasound available (which this service did not have during their study period) may allow for refinement of patient selection.
The larger geography is a challenge we face in the US also, and it may explain why EHAAT had different outcomes from their neighbors in London. The London Air Ambulance group previously published prehospital RT data citing mean times of about 9 minutes to get to scene and an 18% survival to hospital discharge in their penetrating trauma group (with 85% having a good neurologic outcome). Ultimately prolonged transport times mean a further delay of getting the patient to the operating room (OR), but conversely argue in favor of providing the intervention on scene, if able. By the time the patient got to the hospital without any intervention, it would definitely be too late.
However, prolonged transport times are not strictly a rural versus urban problem: dense urban environments significantly increase prehospital times also. An important part of using helicopters in these services is to rapidly insert the critical care asset on scene, and this paper shows the teams arrived reasonably rapidly. Most of the transported patients were however moved by ground. I would argue that given the severity of the injuries, the physical distance, and the higher likelihood of needing a Major Trauma Center’s resources, air transport could have been considered instead, in conjunction with a direct-to-OR approach. This group actually cites an instance where the resuscitative thoracotomy was performed on the helicopter, and thus likely they should be able to transport an open-chest patient on this platform also.
Interestingly, almost half the blunt trauma patients had cardiac output on arrival of the HEMS team. I reached out to the first author to see whether these patients just rapidly arrested on the team’s arrival or whether the arrest was preceded by another intervention such as prehospital emergency anesthesia. Certainly, our own in-hospital practice has changed significantly in recent years as we have become acutely aware of the potentially disastrous effects of administering induction agents and positive-pressure in patients with severe hemorrhagic or obstructive physiology. Reviewing his additional data does show that the teams carefully sequenced their resuscitations including adjustment of medication dosages and the use of blood products in later cases. One must remember however the challenges of working in the prehospital environment when multiple simultaneous interventions may be required of a limited number of personnel on a patient who is rapidly circling the drain.
Finally, this paper reaffirms that blunt trauma patients suffer much more diffuse energy transfer and injury than from penetrating trauma mechanisms. Although a much higher than expected number had a tamponade, none of these patients ultimately achieved ROSC or survived if they did have ROSC. This likely indicates that these patients may not have their problem “fixable” at scene, although if a tamponade is present, it makes perfect sense to relieve that. EHAAT’s operating guidance even states:
“resuscitative thoracotomy in blunt trauma has a very poor prognosis. There is a move in-hospital to limit this to patients who are suspected to have arrested due to an underlying chest injury. For example, multiple left sided rib fractures with suspected penetrating cardiac injury/tamponade, or sudden anterior/posterior deceleration injury to the chest with risk of IVC tear or atrial appendage blow out.”
Is it then futile to perform resuscitative thoracotomy in the prehospital setting outside of an area with much shorter scene arrival and transport times? Perhaps. To me, this paper provides some key insights to be able to achieve marginal gains within systems that are challenged by these limitations. Ultimately, the ability to get a critically injured patient with an output to the hospital, even if they don’t ultimately survive, has benefits in terms of the ability to salvage organs for donation, and importantly to allow a family to see their loved one a final time.
Thanks to EHAAT’s Phillip Almond (@philalmond5) for putting the paper together and for providing me additional unpublished information about the patients he and his team cared for.
vb
Zaf
References
Almond P, Morton S, OMeara M, Durge N. A 6-year case series of resuscitative thoracotomies performed by a helicopter emergency medical service in a mixed urban and rural area with a comparison of blunt versus penetrating trauma. Scand J Trauma Resusc Emerg Med. 2022 30(1):8 https://pubmed.ncbi.nlm.nih.gov/35081989/
Davies GE, Lockey DJ. Thirteen survivors of prehospital thoracotomy for penetrating trauma: a prehospital physician-performed resuscitation procedure that can yield good results. J Trauma. 2011;70:E75–8. https://pubmed.ncbi.nlm.nih.gov/21131854/
Harvin JA, Maxim T, Inaba K, et al. Mortality after emergent trauma laparotomy: a multicenter, retrospective study. J Trauma Acute Care Surg. 2017 83(3):464-468. https://pubmed.ncbi.nlm.nih.gov/28598906/
Marsden M, Carden R, Navaratne L, et al. Outcomes following trauma laparotomy for hypotensive trauma patients: A UK military and civilian perspective. J Trauma Acute Care Surg. 2018 85(3):620-625. https://pubmed.ncbi.nlm.nih.gov/29847536/


Quote from the original paper: “Currently, ultrasound to look for cardiac tamponade is not part of the SOP for RT in our service and this too may be something that should be included in the future”.
Can anyone please give me a good reason why NOT to look with ultrasound before cracking someone’s chest open for suspected cardiac tamponade, ESPECIALLY in prehospital environment???? Of course, it’s a rhetorical question…
Furthermore they write: “It is interesting to note that, in one of the penetrating patients the indication for RT was for aortic control and not to exclude tamponade…” So it means that “exclusion of tamponade” is an indication for the majority of their RT’s? In XXI century, when ultrasound fits in your pocket, you’d do prehospital RT to exclude tamponade instead of POCUS? As an EMS doc… I am speechless…
Interesting Kasia. I think if you have USS immediately to hand, turned on, plugged in, and you’re not doing anything else (or you have multiple people) then it seems like a reasonable action. However, in practice, and especially in teams that are not used to this sort of scenario you can see a lot of wasted time whilst people faff about with kit/views/interpretation in what is an extremely time critical condition.
Another situation may be the patient who clearly has a stab/bullet wound directly over the heart and is periarrest/arrest. How. much value would USS add in that situation?
There is also the issue of surgical emphysema obscuring views which can happen in some circumstances.
So….. if well drilled and skilled and equipped and staffed you may remain speechless. In other circumstances it may not be as clear.
My personal view is to use USS in hospital when it is likely to be useful and/or in circumstances of uncertainty, but defo not in every case. In the prehospital environment we are just starting to use USS as recently acquired for CSI BASICS/NWPCCC https://www.csibasics.org.uk/
S