This week I am in Jeddah at the Saudi Arabian Society of Emergency Medicine1. It has been a fabulous few days so far. The content is good, the presentations are way above average and I’ve been looked after superbly. You could not ask for better hosts as an international speaker and I’m honored to have been invited. Jeddah is a beautiful place too. It’s warm, friendly and has one of the finest sunsets I’ve seen in the world. I’ve learned so much about Saudi Arabia and the 2030 vision for the country and in truth some of my assumptions have been challenged.
From a personal perspective this has been a journey back to the Middle East from my youth. When I was 15 my parents moved to Dubai (well before it was the international metropolis it is today) and so I remember this part of the world well, but this is the first time I am returning for any length of time. Jeddah today reminds me of the great times I’ve spent in the Middle East. This is a great place and if you get the opportunity to visit or to attend SASEM in the future I would recommend you do so. This is a great place to visit and learn.
The aim of this blog is to link the 10+1 papers I’m talking about on day 2 of the conference. We’ve talked about these on the blog before but I thought it might be helpful to put them in one place so that we can distribute them to delegates for future reference.
Choosing which papers are the ‘Top 10’ is obviously an entirely imprecise art. I’ll let you into my secret…….., they are basically the ones that are related to resus room/critical care elements of emergency medicine that interested me over the last year and which either have changed my practice OR are likely to change my practice in the near future.
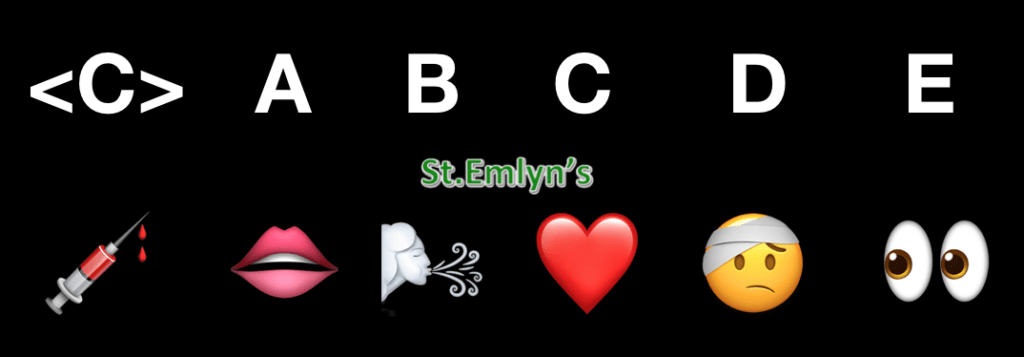
Just for fun (and after I did something similar at the ICSSOA conference, I’ve taken the theme of emojis to subdivide the papers into the CABCDE system.
Paper 1. PAMPER trial

Paper 1 is the PAMPER trial that looked at the use of prehospital plasma in patients suffering major trauma. The idea here is that we need to manage coagulopathy in the seriously injured and by getting ahead of the curve by giving FFP early. This large RCT based in the US showed a 9.8% increase in survival which is incredible. It is the sort of treatment effect that is so large that I’d like to see it repeated. You can read more about the PAMPER trial on the Bottom Line Website here.2,3

Paper 2: Airways-2
Paper 2 is the AIRWAYS-2 trial that compared the use of supraglottic airways vs Intubation as the primary airway device in patients with out of hospital cardiac arrest. This large (over 9000 patients) RCT conducted in the UK failed to demonstrate any significant difference between the two devices. The authors looked at the results on an intention to treat basis, and also on a pragmatic analysis and neither approach demonstrated an advantage.

There are a few caveats in this study when we think about applying it to the ED. Firstly this trial is about initial airway approach and clearly in patients who recover, but who do not wake up then intubation will be required for ICU care. We also need to think a little about ETT use and ask ourselves whether a paradox may occur that if an ETT is a better airway it might result in excessive ventilation (which is bad). This is discussed in more depth in our previous blog on this trial and also on the PART trial from the US which came to the same conclusion.4,5
Paper 3: Superoxia in the critically unwell patient.
Paper 3 is a systematic review of the use of oxygen in the critically ill patient. Over the years there has been lots of work looking at the potential harms of supranormal levels of oxygen in critically ill patients and in general wherever it has been looked at there has been little evidence of benefit and sometimes of harm.

This paper brings together 25 studies across a range of unwell patients to look at whether a restrictive (SaO2 92-96%) vs a liberal strategy (whatever you like) makes a difference to patient outcome6,7. The bottom line here is that it does. Although the NNT is reasonably large (about 100 for final outcome), the sheer number of patients undergoing treatment means that this may have a big effect across a health care economy. Read more here about why we should all be using a restrictive practice.
Paper 4: Bougie use in the ED
Paper 4 is an RCT comparing the routine use of a bougie in the ED against the use of a stylet. This is an important study for me as I’ve advocated the routine use of a bougie for as long as I can remember. However, others have suggested it takes more time, that it might cause injury or that a stylet (or nothing at all) is better.

This paper demonstrates that not only is the bougie safe, but also that it is quicker and easier to use. This is true irrespective of whether you think it’s going to be a difficult airway. The bottom line is use a bougie in most cases.6–9
Paper 5: Conservative management of pneumothoraces
In this ED based study of reasonable size the authors showed that the bougie is better in terms of time, ease and success. There was no suggestion of injury either. The bottom line for me is to routinely use the bougie when intubating in the ED.

This paper looks to whether it is safe to observe some traumatic pneumothoraces. It’s important to me as I’m older enough to remember a time when any traumatic PTX got a chest drain, and especially those who were going to go onto IPPV. In truth that was based on the chest Xray which meant that we probably (Ed- inevitably) missed some of them and got away with conservative management through ignorance as much as anything else. In the modern age the routine use of CT in trauma has led to a much greater number of pneumo and haemothoraces being diagnosed. If we carry on the mantra of every PTX/HTX needing a drain then that would mean a lot of drains! Whilst I like putting in drains, it’s not great for patients as there is a clear morbidity associated with them.
In this paper from a single UK trauma centre the evidence suggests that if you decide to manage a PTX/HTX conservatively then that decision is safe and likely to work 90% of the time even if the patient is on IPPV10,11. Read more on the blog here.
Paper 6: Epinephrine in cardiac arrest.
The paper we were all waiting for. Does epinephrine (Ed- you mean Adrenaline really 😉 ) make a difference. The answer is more complex than the question. In this large UK based prehospital RCT the answer is that more people survive but at the expense of a much greater number of patients with severe disability.

So that leaves us with a dilemma. Is the small number of survivors worth it? I think this is a question for society rather than medicine as I can’t really get my head round it. At the moment ILCOR has recommended we keep using it, but whether things stay that way is uncertain. Read more on the blog here.12,13
Paper 7: Hypothermia in head injury
Hypothermia should work for lots of critical illness, but it doesn’t seem to in practice. Whilst lab data suggests and demonstrates the neuroprotective effect of hypothermia we’e failed to demonstrate it in several different areas (notably post cardiac arrest). What about head injury though? On the ICU the Eurotherm trial showed that it did not make a difference in patients with raised ICP, but that was criticised as the hypothermia was started late. What happens if we start it early?

In the POLAR trial patients were randomised as soon as possible to hypothermia after head injury. In this large RCT there was little difference in outcome and more complications in the hypothermia group. Once again hypothermia fails to live up to the promise although it’s still unclear why. Read more on the blog here.14,15
Paper 8: Neurofilaments in cardiac arrest prognosis.
Predicting outcome post ROSC following cardiac arrest has always been difficult. Clinicians have used many signs and features to estimate prognosis but it’s always been difficult and as the TTM trial showed, especially difficult in the early stages.

Neurofilament light chains are something you might not have heard of, but think of them as potential troponins for the brain. In essence they are released from damaged brain tissue.
In this sub analysis of the TTM trial16 the authors looked at whether these neurofilaments can predict outcome from cardiac arrest and the answer seem to be that they are far better than anything else we have17. This could be a real game changer in cardiac arrest and although not yet ready for prime time might be the first we have that can rule in and rule out good outcomes. I’m also interested to see if this analysis will be used in future studies of other neuro problems such as stroke and trauma. Watch this space! Read more here.18
Paper 9: Contrast and CT scans.
Does contrast cause AKI in patients undergoing CT scan? Well this paper has been shared widely but I make no apology for re-iterating it as it has not made the leap into many radiology departments as yet.

In an observational study of ED patients undergoing CT scans in the ED, the use of contrast does not make a difference to renal outcomes. The bottom line is that the underlying condition is far more likely to cause renal failure than the use of contrast. If your patient needs a CT – just get on with it and worry about dialysis later. Read more here.19,20
Paper 10: The end of the ‘roid
Steroids seem to come and go as frequently as the tide. Some weeks they are the best thing ever, then they are awful. It’s tricky to keep up…. We now know that they are ineffective in head injury and spinal injury, but what about sepsis? The routine use of steroids has been in and out of fashion for years but now we have definitive evidence.

In this large RCT based in Australasia they showed that there is no difference in the routine use of steroids in septic shock. So unless there is a specific reason (eg recent steroid use) then keep the hydrocortisone in the cupboard. Read more here.21,22
Paper 10+1: The Zero Point Survey
Cheekily I added the zero point survey paper that I co-authored in 2018. Why you may ask? It’s because of all the things I’ve done this year it’s the easiest, quickest, cheapest and most effective to deliver in practice.

We don’t have the evidence yet, but it makes sense and I’d strongly recommend you consider putting it into your practice. Read more about the ZPS here.23,24
Final thoughts
I’ve another day here in Jeddah and another presentation to come. I’ll soon be back in the UK, wiser, happier, and enthused to get back to work in Virchester thanks to my SASEM hosts.
vb
S
References
- 1.SASEM2019 – SASEM. Saudi Society of Emergency Medicine. https://sasem2019.com/. Published September 12, 2014. Accessed February 5, 2019.
- 2.PAMPer. The Bottom Line. https://www.thebottomline.org.uk/summaries/em/pamper/. Published August 3, 2018. Accessed February 5, 2019.
- 3.Sperry JL, Guyette FX, Brown JB, et al. Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock. N Engl J Med. 2018;379(4):315-326. doi:10.1056/nejmoa1802345
- 4.Liebig A. JC: OOHCA and Airway management. Do we need a tube? St Emlyn’s • St Emlyn’s. St.Emlyn’s. http://www.stemlynsblog.org/jc-oohca-and-airway-management-do-we-need-a-tube-st-emlyns/. Published September 2, 2018. Accessed February 5, 2019.
- 5.Benger JR, Kirby K, Black S, et al. Effect of a Strategy of a Supraglottic Airway Device vs Tracheal Intubation During Out-of-Hospital Cardiac Arrest on Functional Outcome. JAMA. 2018;320(8):779. doi:10.1001/jama.2018.11597
- 6.Carley S. JC: Oxygen in the Acutely Unwell Patient. St Emlyn;s • St Emlyn’s. St.Emlyn’s. http://www.stemlynsblog.org/jc-oxygen-in-the-acutely-unwell-patient-st-emlyns/. Published May 13, 2018. Accessed February 5, 2019.
- 7.Chu DK, Kim LH-Y, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. The Lancet. 2018;391(10131):1693-1705. doi:10.1016/s0140-6736(18)30479-3
- 8.Driver BE, Prekker ME, Klein LR, et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation. JAMA. 2018;319(21):2179. doi:10.1001/jama.2018.6496
- 9.Carley S. JC: Don’t blame it on the Bougie. St Emlyn’s • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/jc-dont-blame-it-on-the-bougie-st-emlyns/. Published May 20, 2018. Accessed February 5, 2019.
- 10.Walker SP, Barratt SL, Thompson J, Maskell NA. Conservative Management in Traumatic Pneumothoraces. Chest. 2018;153(4):946-953. doi:10.1016/j.chest.2017.10.015
- 11.Carley S. JC: Conservative management of chest trauma. St Emlyn’s • St Emlyn’s. St.Emlyn’s. http://www.stemlynsblog.org/jc-conservative-management-of-chest-trauma-st-emlyns/. Published December 7, 2018. Accessed February 5, 2019.
- 12.Perkins GD, Ji C, Deakin CD, et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018;379(8):711-721. doi:10.1056/nejmoa1806842
- 13.Carley S. JC: Does Epinephrine work in Cardiac Arrest. St Emlyn’s • St Emlyn’s. St.Emlyn’s. http://www.stemlynsblog.org/jc-does-epinephrine-work-in-cardiac-arrest-st-emlyns/. Published July 19, 2018. Accessed February 5, 2019.
- 14.Horner D. JC: Hypothermia in brain injury: The POLAR trial. St Emlyn’s. • St Emlyn’s. St.Emlyn’s. http://www.stemlynsblog.org/jc-hypothermia-in-brain-injury-the-polar-trial-st-emlyns/. Published November 3, 2018. Accessed February 5, 2019.
- 15.Cooper DJ, Nichol AD, Bailey M, et al. Effect of Early Sustained Prophylactic Hypothermia on Neurologic Outcomes Among Patients With Severe Traumatic Brain Injury. JAMA. 2018;320(21):2211. doi:10.1001/jama.2018.17075
- 16.Carley S. JC: What’s the target temperature for OOHCA cooling. St.Emlyn’s • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/whats-target-temperature-oohca-cooling-st-emlyns/. Published November 18, 2013. Accessed February 5, 2019.
- 17.Moseby-Knappe M, Mattsson N, Nielsen N, et al. Serum Neurofilament Light Chain for Prognosis of Outcome After Cardiac Arrest. JAMA Neurol. October 2018. https://www.ncbi.nlm.nih.gov/pubmed/30383090.
- 18.Horner D. JC: Do you see the light? Serum neurofilament light chain for prognostication following OOHCA • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/jc-do-you-see-the-light-serum-neurofilament-light-chain-for-prognostication-following-oohca/. Published January 13, 2019. Accessed February 5, 2019.
- 19.Hinson JS, Ehmann MR, Fine DM, et al. Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Annals of Emergency Medicine. 2017;69(5):577-586.e4. doi:10.1016/j.annemergmed.2016.11.021
- 20.Carley S. Top 10 trauma papers 2017-2018 for @traumacareUK conference. St Emlyn’s • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/top-10-trauma-papers-2017-2018-for-traumacareuk-conference-st-emlyns/. Published April 18, 2018. Accessed February 5, 2019.
- 21.Horner D. JC: The End of the ’Roid? ADRENAL • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/the-end-of-the-roid-jc-adrenal/. Published January 22, 2018. Accessed February 5, 2019.
- 22.Venkatesh B, Finfer S, Cohen J, et al. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. N Engl J Med. 2018;378(9):797-808. doi:10.1056/nejmoa1705835
- 23.Reid C, Brindley P, Hicks C, et al. Zero point survey: a multidisciplinary idea to STEP UP resuscitation effectiveness. Clin Exp Emerg Med. 2018;5(3):139-143. doi:10.15441/ceem.17.269
- 24.Carley S. JC: The Zero Point Survey. Optimising resuscitation teams in the ED. St Emlyn’s • St Emlyn’s. St.Emlyn’s. https://www.stemlynsblog.org/jc-the-zero-point-survey-optimising-resuscitation-teams-in-the-ed-st-emlyns/. Published September 30, 2018. Accessed February 5, 2019.


Pingback: February 2019 Podcast round up: St Emlyn's • St Emlyn's